Découvrir les récits sur la façon dont les troubles de la coagulation ont impacté certaines personnes et leurs proches
Le contenu publié sur ce site a été soumis par des tiers et n’est ni représentatif ou approuvé par la Fédération mondiale de l’hémophilie.
Speaking Up for China’s Women with Hemophilia: My Story and Theirs
As the daughter of a man with hemophilia, a woman with mild hemophilia myself, and a former sufferer of heavy menstrual bleeding, I cannot remain silent after discovering the vast gap in awareness and care for women with hemophilia in China.
For 18 years, I never suspected that I might have a bleeding disorder—largely because China’s public education and medical resources on hemophilia are outdated, school textbooks still claim that female carriers never show symptoms. I dismissed my heavy periods as normal and ignored signs like frequent bruising and bleeding gums.
It wasn’t until I came across educational materials from the World Federation of Hemophilia (WFH) that I learned: carriers can indeed be patients.
At 18—seven years after my first period—I used the PBAC method for the first time and found I was losing 200 mL of blood every cycle.
At 18—after living with symptoms for 18 years—I took the BAT bleeding assessment and scored a 7.
At 18—just ten minutes before entering surgery for appendicitis—I had my clotting factor levels tested for the first time, discovering they were only at 12%. The surgery was immediately halted.
At 18—I knew for the first time that, I was, in fact, a person with hemophilia.
And I know I am not alone.
Since April 2024, I’ve been traveling across China giving talks and meeting other women with hemophilia.
Many of them do not speak English, cannot use computers, and have never shared their stories—yet their suffering deserves to be heard.
Today, I would like to share the voices of women in China with WHD stories.
Her body had been crying out for help for years, but no one listened—until she nearly lost her life on the delivery table.
She had always bruised easily, bled from her gums, and had wounds that took too long to heal. These symptoms were dismissed as “just being weak.”
Her first challenge came during the birth of her older son. The bleeding was significant, but her concerns were brushed aside:
“That’s just childbirth—it’s normal to bleed,” the doctors said.
Her son was later diagnosed with hemophilia, and she quietly shouldered the burden of care.
Years later, she had a second son via C-section at a county hospital.
She told the doctor: “My older son has hemophilia—should I be worried?”
The doctor replied: “You’re just a carrier. It’s fine.”
It wasn’t.
That night, blood began pouring from her surgical wound. Her bedsheets were soaked.
Panic broke out. The hospital lacked experience and resources.
She remembers hearing her name faintly through a haze, as she slipped in and out of consciousness.
Later, she learned that she had been issued a critical condition notice.
The wound had split open, and the hospital—unprepared and without coagulation factor VII concentrate—barely saved her life using whole blood transfusion.
Only after this traumatic experience did she discover: her own clotting factor was around 20%.
She, too, was a person with hemophilia.
Later, when she needed heart surgery, she knew she required clotting factor.
But unlike male patients, she could not receive insurance reimbursement. The medication would cost over 100,000 RMB(13,870 USD) out-of-pocket, more than her yearly income.
Looking back, she said:
“Every time a doctor dismissed my concerns, every time I got lucky, it was my life they were gambling with.”
One girl from northern China wore thick cotton pants in winter—yet her legs were always covered in large bruises.
Another, from the south, loved jump rope and dancing—but was constantly sore and bruised after play.
The northern girl told herself the blood when brushing her teeth was “just sensitive gums.”
The southern girl thought her childhood nosebleeds were just clumsiness.
Both were anemic and fatigued. Both were told: “It’s just your constitution—be strong.”
Both daughters of hemophiliacs. Both thought they were alone.
Until one day, they met—and realized they shared the same invisible story.
They talked about hiding their symptoms from family, doctors who said: “You’re just a carrier—nothing to worry about,” and the shame they felt about needing accommodations in dating, work, and life.
The northern girl feared hospitals—until she fainted from iron-deficiency anemia(IDA).
The southern girl actively sought care—yet most doctors had never heard of women with hemophilia.
The northern girl used 25 daytime and 6 nighttime pads per cycle. She had to wake up at night to change them.
The southern girl regularly stained clothes and bedsheets, experiencing dizziness and exhaustion during her period.
When they finally estimated their blood loss using PBAC:
The northern girl lost 187 mL per cycle, she lost 85% of her body’s blood volume yearly—equivalent to 4.8 bottles of 500mL
The southern girl lost 203 mL, lost 92% yearly—that’s 5.2 bottles.
The northern girl never tested her factor IX level.
The southern girl tested her factor VIII—only 19%.
They were not merely “carriers.”
They were women with hemophilia.
“I can’t run or play soccer. If I get hit on the head, it could be very dangerous.”
—Ningning, 7 years old, diagnosed with Factor VII deficiency
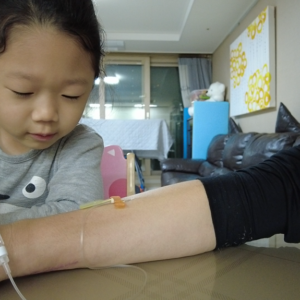
We met Ningning, a bright, cheerful first grader who loves drawing(image attached).
She enjoys light games like hopscotch and tag—but knows not to do anything that might cause bleeding.
At age 3, she had a nosebleed that lasted two days, ending in a collapse.
Her parents were sent from county to city hospitals, only finding help in a major hospital in Guangzhou.
Her mother recalls: “There was so much blood, it even came out of her eyes.”
Ningning was diagnosed with a rare bleeding disorder: Factor VII deficiency. Since then, her family has faced tremendous pressure.
The targeted treatment—Factor VII concentrate—is not yet produced in China. The only available option is an imported American drug, priced at 5,000 RMB per dose(693 USD), equivalent to the family’s entire monthly income.
Unable to afford this regularly, they turned to a cheaper alternative: a domestic “complex concentrate”, costing a few hundred RMB per dose.
It is less effective and comes with greater side effects—but with no domestically approved Factor VII yet available, they had no other choice.
Ningning is used to injections now. She says: “It doesn’t hurt if I stay still.”
She’s braver than many adults—but she shouldn’t have to be.
She is one of hundreds of thousands of girls and women with bleeding disorders in China, still too “invisible”—to doctors, to insurance systems, to society.
They long to run, dance, and go to gym class—but they need more awareness, compassion, and policy change.
Tingting’s very first period was a crisis. She bled so heavily she couldn’t stay in class.
The blood soaked her seat. She nearly fainted.
She was hospitalized and eventually diagnosed with rare Factor VII deficiency.
Now, every month, she needs injections to control the bleeding.
She’s traveled from hospital to hospital, relying on medication just to live a normal school life.
But after physical activity—running or sports—she suffers severe joint and muscle pain.
No matter how hard she trains, she’s unable to complete her physical education exam.
Her mother says:
“She’s academically strong, but missing 20 points in the high school entrance exam’s PE section might ruin her chances.”
They’ve tried hormonal treatments, but the side effects were too severe.
Now, she comes home after school during her period to receive clotting injections.
When clinics refused to administer the shots, her mother learned to do it herself.
“I’m better than the nurses now,” she jokes.
Their fridge is filled with medicine, not food.
Each vial costs hundreds of RMB. She needs over ten a month. None are covered by insurance.
These stories represent only a fraction of the women I’ve met. They are strong, but they should not have to suffer in silence.
Girls and women with bleeding disorders have long been overlooked in global care systems, and even more so in countries where diagnostic and treatment resources are limited.
In China, many are still undiagnosed, misdiagnosed, or under-treated simply because of their gender.
We established a organization named WGH38417 in China. You could see our efforts at our website. Contact me via Reddit.
We call on the global bleeding disorder community—researchers, clinicians, policy advocates, and patient leaders—to:
The title for 2025 Hemophilia day is ‘Access for all: Women and girls bleed too’.
Let her be heard. Let her be diagnosed. Let her be safe.
MD MOMINUL HOQUE
Founder, Disabled Rehabilitation Foundation (DRF), Dhaka, Bangladesh
Executive Director, Uttara General Hospital Ltd., Uttara, Dhaka, Bangladesh
Chairman, Mayer Hasi General Hospital, Ashulia, Dhaka
At the Disabled Rehabilitation Foundation (DRF), we believe that every individual, regardless of physical ability or financial condition, deserves access to quality healthcare and rehabilitation. Our journey began with a vision—to create a society where persons with disabilities receive the support, care, and opportunities they need to lead independent and fulfilling lives.
Since the year 2015, we have been working regularly with hemophilia patients. Our organization, DRF (Disability Rehabilitation Foundation), has so far been providing medical support to a total of 170 hemophilia patients. The treatment expenses have been managed through personal initiatives and with funding from the DRF Foundation.
In particular, we have been purchasing Factor VIII and Factor IX to provide the necessary treatment to patients. However, bearing these expenses is becoming increasingly difficult for us.
We believe that if the World Federation of Hemophilia (WFH) provides us with factor support, it will serve as a significant financial and emotional relief for our patients. This assistance will help ensure continuous and effective treatment for them.
On this WHD (World Hemophilia Day) 2025, I wish all hemophilia patients around the world good health and a bright future.
We sincerely hope that WFH will stand by us and extend its support in this regard.
Regards
Md Mominul Hoque

Living with Hemophilia, Thriving with Hope!
My name is Siam Ahmed, and 15 years old. Since birth, my life has been a little different – I was born with a rare bleeding disorder called Hemophilia-A. Even a small cut can lead to prolonged bleeding. When I fall while playing, others get up and carry on, but for me, it can turn into a serious and painful ordeal. The bleeding doesn’t stop easily, and the pain is often so intense that it keeps me awake at night.
My family’s financial situation is modest. I have no father, 5 years ago he is died of road accident. My mother is a laborer. The treatment for Hemophilia is expensive – I regularly need a medication called “Factor VIII” to help my blood clot. Unfortunately, I couldn’t always afford it. There was a time, when I truly believed this condition would bring my life to a halt.
That’s when the DRF Foundation (DRF) became my light in the darkness.
DRF Foundation (DRF) didn’t just support me with medicine – they reminded me that I wasn’t alone. They covered the cost of my treatment, arranged regular medical follow-ups, and even supported my education. Their kindness and commitment gave me strength. Because of them, I can now attend school regularly, and more importantly, I have begun to dream again – to imagine a future where I can grow up and help others, just as DRF Foundation (DRF) has helped me.
Hemophilia is a part of my journey, but it doesn’t define who I am. DRF Foundation (DRF) helped me discover the courage to say, “Yes, I can.”
Thank you, DRF Foundation (DRF) , for standing beside me when I needed it most. You didn’t just support my health – you restored my hope.
Hey! I’m Devang, 23, from India. I do freelance social media marketing, which lets me work from home on my own terms. Alongside that, I’m also preparing for government services—that’s the long-term goal.
As a kid, I was super active. But because of low Factor VIII levels, I had to deal with a lot of internal bleeds—some pretty scary, even life-threatening… I remember being in hospital for months multiple times when i was a kid. Still, thanks to my parents’ support and resilience, I managed to have a pretty healthy and active teenage life.
In the last 6–7 years though, things changed. I developed severe target joints, and honestly, it’s impacted my life in more ways than I can count. That constant feeling of weakness, of not being able to do what others around you can… yeah, I know that feeling too well.
But here’s the thing—I don’t see it as a struggle. It’s a fight. Every single day. With the condition, with its complications, and everything it tries to take from you.
What’s helped me? Staying informed. Learning about treatments and management. Being part of the community—online and offline. Talking to doctors regularly. Staying in touch with my local HTC and haemophilia chapter.
Because of all that—and the people around me—I’ve been able to keep my joints working pretty well. No major deformities so far. Yes, I’ve got haemophilic arthropathy too, like many others. But trust me, there’s always a way to move forward and that’s what I’m doing currently! Fighting my way out to more healthy joints.
You’re not alone in this. Keep learning, keep fighting, and most importantly—keep showing up.
If you wish to connect, my email is: devangagarwal0211@gmail.com
Professor of Hematology
Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
HTC, Chairman- Lab One Foundation & Director, WBDR- HTC (BSMMU)
We are currently providing care and support to over 800 registered hemophilia patients through our Hemophilia Treatment Centers (HTCs) at BSMMU and Lab One Foundation. Our services include outpatient, inpatient, and emergency care facilities tailored specifically for individuals living with hemophilia.
Most of the treatment factors we administer are generously provided through the Humanitarian Aid Program of the World Federation of Hemophilia (WFH). Due to the limited supply, implementing a prophylaxis protocol remains a challenge in our HTCs. We sincerely appreciate WFH’s continued support through factor donations and the WBDR HTC Support Awards, which are invaluable to our operations.
Our dedicated HTC nursing staff regularly participates in online training programs organized by the WFH WBDR team, which has significantly enhanced the quality of care we provide.
We proudly celebrated World Hemophilia Day (WHD) 2025 through a series of impactful events. These included an awareness rally, a scientific session, and a round-table discussion involving key stakeholders such as the Rotary Club, Director General of Health Services, Ministry of Health, university authorities, social workers, and representatives from print and electronic media.
I am honored to serve as the Chief Coordinator for the development of the National Hemophilia Guideline, which has now been finalized and is awaiting official declaration.
The Government of Bangladesh has also extended support in purchasing clotting factors for selected government HTCs. However, HTC, BSMMU and HTC, Lab One Foundation (LOF) are non-governmental organizations and thus rely entirely on humanitarian aid and philanthropic contributions. HTC LOF operates 24/7 with full emergency facilities, including a blood bank, laboratory, operating theatre, and a dedicated team of doctors, nurses, and support staff.
One of our patients, Sadian, a 17 years old with Hemophilia A who has developed inhibitors, is currently receiving treatment with Emicizumab.
Given our ongoing needs and the rising number of patients, I would like to kindly request WFH to consider extending their support further through factor donations and WBDR HTC Support Awards.
We remain hopeful that World Hemophilia Day 2025 will mark a new era in ensuring access for all, especially in line with WFH’s current focus on bleeding disorders in women and girls.
Warm regards,
Prof. Dr. Md. Salahuddin Shah
Professor of Hematology
Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
I am Khandaker Amirul Islam, Haemophilia – A patient working as a volunteer & patient counselor of HTC Lab One Foundation. My WBDR ID number is 28569, HTC Lab One Foundation, Uttara – 1230, Dhaka, Bangladesh.
@Success History@
Last four months ago, suddenly I felt severe chest pain & attended at HTC LOF. I was a regular attendee for my routine follow up at HTC Lab One Foundation under Professor Dr. Md. Salahuddin Shah.
He arranged for my admission under his supervision at BMU ( BDMMU). And finally after angiography I had been got two heart rings implanted in my heart from Cardiology Department of Bangladesh Medical University (BSMMU).It was a very difficult task for me and it was not so much easy that it could be done from any place but by the grace of Almighty Allah Prof.Dr. Md. Salahuddin Shah & Cardilogy Department helped me a lot. I have received required factors from HTC LOF, HTC BSM ( BSMMU) & NMO (HSB). Fortunately my life is safed. I am grateful to WFH Humanitarian Aids HTCs & HSB.
Now I have to take Factor Vlll after every 15 days.
Most of the haemophilia patients in our Country are very poor. So we need increased number of factors for our survival.
We have observed World Hemophilia Day 2025 through rally, Scientific seminar & patients counselling at HTC LOF.
I sincerely appeal to the WFH Humanitarian Aid & WBDR team to consider allocating more clotting factors to HTC, Lab One Foundation & this HTC remained open for 24 hours.
I believe this will enable the organization to save the lives of many more hemophilia patients and continue to provide compassionate support to them.
On this special day, I wish all hemophilia patients around the world good health and a bright future.
My son Owen has severe Hemophilia, today my office show support and love. Team Owen!!!

I am Hafizur Rahman, WBDR Data Management and Patients Councilor, HTC, Lab One Foundation, Dhaka, Bangladesh.
From my professional experience, I have closely observed the sincere and selfless efforts of the Honorable Sir Prof. Dr. Md. Salahuddin Shah, Chairman of Lab One Foundation, who has always stood beside hemophilia patients. He has been relentlessly working to ensure their healthy lives by providing free treatment, essential medicines, fresh frozen plasma, and clotting factors.
Through regular communication with patients and listening to their stories of daily struggles, I have come to realize the immense battle they fight every day just to survive and stay healthy. Especially when unexpected bleeding occurs in any part of their body, Lab One Foundation, always remains prepared to provide the necessary medicines, factors, and fresh frozen plasma as swiftly as possible.
I would like to express my heartfelt gratitude and deep respect to the Honorable Sir Prof. Dr. Md. Salahuddin Shah, Chairman and the entire team of HTC, Lab One Foundation, for their compassionate and humanitarian efforts.
On the occasion of World Hemophilia Day 2025, I sincerely appeal to WBDR to kindly consider the allocation of clotting factors to HTC, Lab One Foundation, . I believe this will enable the organization to save the lives of many more hemophilia patients and continue to extend its compassionate support to them.
On this special day, I wish good health and a bright future to all hemophilia patients around the world.

“A Silent Bleed, A Silent Loss”
As a Clinical Haematologist dedicated to serving patients with bleeding disorders, I often meet individuals whose lives have been shaped by unrecognized or untreated conditions. Recently, I encountered a deeply moving case that reminded me how crucial awareness and early diagnosis truly are.
A young woman was admitted to the gynaecology ward during her first postnatal period with uncontrolled bleeding from a surgical wound following an emergency hysterectomy. Her story unfolded tragically: after a Caesarean section, excessive bleeding began and could not be controlled even after uterine closure. The obstetric team, in a desperate attempt to save her life, had no choice but to perform a hysterectomy.
When I was consulted, I delved deeper into her medical history. She revealed she had experienced heavy menstrual bleeding (menorrhagia) since menarche. Yet, due to social stigma and lack of awareness, neither she nor her family ever sought medical advice. Her symptoms were normalized, explained away by vague cultural beliefs and silence.
Unfortunately, that silence cost her dearly—her ability to become a mother was taken away in a moment that should have brought her joy. What could have been managed with timely diagnosis and care turned into irreversible loss.
This story is a painful but powerful reminder: bleeding disorders in women are underrecognized, under diagnosed, and often hidden behind shame or misinformation. We must speak up, educate, and ensure that no one loses their future to a treatable condition.
On this World Hemophilia Day, let us reaffirm our commitment to break the silence, raise awareness, and advocate for early diagnosis and care for all—especially the women and girls who bleed unseen.

“Strengths with Deficiency”
I’m not writing about my so called Royal Disease clotting factor😁, it’s about those moments which are almost deficit from my life, maybe it’s the feeling of majority persons with bleeding disorders.
Your childhood will be ruined by your pressurized limited life, your special events like Eid, Christmas and Diwali or even marriages.
I missed my school life I wish to be punished by my teacher but because of my family doctor they don’t allow my teachers to punish me, i never like to be special (sympathy)boy.
But when the creator take something from you he gives you extra strengths like, Endurance you will not take painkillers for your pain because you knew that, it will not work on your severe pain.
You will always be Aware of coming struggles and your survival strategies.
Sometime there will be nothing left for the cure, but you will Fight like warrior.
Whenever you felt tired in your life you will find your Parents beside you. It’s the beautiful climax of everyone life story, but in our (community🩸) life they have a role of doctors, consultant, physical therapist and nutritionist, sometime friend!
“Life will always hit Hard if you hemophiliac or”
Today is World Hemophilia Day
It has been 3 years since my son was diagnosed with severe hemophilia A. The past years were very challenging for us. Knowing that our country have limited knowledge to rare bleeding disorders, it is also hard for us to look for medical practitioners who knows how to infuse for hemophilia patient.
Recently, our son got into a mild accident wherein he accidentally stumbled and hurt his right foot. He is currently in the province that lacks medical care for patient like him. In order for us to get him treated, we connected to HAPLOS Hemophilia Philippines – an organization for patients with bleeding disorder. I called one of the officers and asked help for the members on nearby areas. Several calls and coordination were made, and luckily we were able to find one. The infusion started and right now he is on recovery mode.
Given that our son is a 3 year old boy and a toddler, it is really hard for us to stop him from moving, as he seeks adventures and obstacles. His pain tolerance is so high that he can endure the pain. But despite that, I am so proud of him being so strong and healthy.
As a mother and a carrier of Hemophilia, I also feel symptoms like easily bruising, heavy menstrual and prolonged bleeding and joint pains across my knees. There are days where the pain won’t let me sleep. But overall, I was able to get through with it.
I am so thankful that even in dark days, the HAPLOS Hemophilia Philippines will always be there as a support system (emotionally and mentally) to mothers like me and patients like my son. Ever since we joined the organization, there was not a time that they did not answer all the inquires I had. They helped me and educated me more about this and engaged with different members.
And to my family especially to my husband, I am so thankful that despite our situation, they are always there to help us during the hard times, added by the people around us who supported us in this journey.
Lastly, as we celebrated the World Hemophilia Day, I want everyone to know that this rare bleeding disorder is just around the corner. To share with them what this is and for them to stop judging the Hemophilia Patients that they are limited on the things they can do, and cannot do normal things like other people does.

I found this page while searching about my hemophilia diagnosis.
My Name is Cindy Nogueras, 28, from Puerto Rico. Back in July 2023, while I was unknowing fighting for my life was diagnosed with Hemophilia factor XII also known as HAF deficiency, Hageman factor deficiency, Hageman trait. Factor XII deficiency is a rare genetic blood disorder that causes prolonged clotting (coagulation) of blood in a test tube without the presence of prolonged clinical bleeding tendencies.
It is caused by a deficiency of factor XII (Hageman factor), a plasma protein (glycoprotein).
The condition caused bleeding in my knees which has left me temporarily in a wheelchair, and stiff leg which can’t stretch due to the loss of the meniscus and cartilage.
This condition is also accompanied by agammaglobulinemia, which means I don’t have the protein which creates the immune system, and I will be having infusion for the rest of my life to treat it.
Although I Was mostly in and out of the hospital growing up, no one ever knew why, once I had a bad fall no one couldn’t tell me why my meniscus and cartilage were getting wear out. Until May 2023, I ended up in wheelchair with a bad pain and bad cramp from leg to knee, my rheumatologist sent me to emergency in suspicion of a sepsis on my knee.
I stayed in the hospital for about 19 days, 4 days in emergency room and 15 days up in a room, with many doctors and specialists visiting, from cardiologists, rheumatologists, orthopedics, hematologists, internists, immunologists and there they found my hemoglobin was in 4 and dropping, a bacteria in my blood, the hemophilia and the agammaglobulinemia.
Although I know neither have a cure, and will always be a part of me, I haven’t stopped doing what I love, I go to events of cosplay, work related events, and my photography hobby. Even if I can’t work now at what I got a degree on, I’m happy to be alive and continuing what I’m doing, with my family supporting me through this journey, mentally and physically.
health insurance doesn’t cover everything but we do everything we can to deal with it.

Yo bien agradecida con la lic.laura Paez y la doc.laura villareal de la clínica de hemofilia del hospital universitario.ya once años que mi hijo es atendido ahí ,es una excelente atención con su gran equipo multidiciplinario,nos han enseñado tantas cosas ,de como debemos llevar una buena profilaxis y poder nosotras mismas infundir a nuestros hijos.gracias a su atención podemos llevar una vida normal .

My name is Eliza VanZweden, and I am writing to share my journey as a woman living with Glanzmann’s Thrombasthenia. GT is a rare bleeding disorder caused by a platelet defect in which platelets do not aggregate to stop bleeding.
I was diagnosed shortly after birth in 1999, due to symptoms of birth trauma. My path to diagnosis was certainly more painless than others, as my older brother had already been diagnosed with GT. Growing up, I struggled with many nosebleeds which would often bleed for days. For these and other serious bleeds like throat and GI bleeds, I received many on-demand platelet transfusions in my youth. There are very limited treatment options for GT patients, who are often left to resort to platelet transfusions, Factor VII bypassing agents, or tranexamic acid. There are no prophylactic options available for GT patients currently.
As I grew, I learned about the risks associated with platelet transfusions – they should only be used to stop bleeding in emergency situations due to the risks of developing antibodies. This left me anxious – my only treatment option could become ineffective at any time and fail me in an emergency situation when I need it the most. The trust that all my bleeds will be solved with a platelet transfusion was replaced with worry surrounding every bleed and debating every time I bleed how much is “too much” before I go in for treatment – does a nosebleed need to last 8 hours before getting a transfusion? Or should it be reserved for one that is bleeding for 4 days?
As I transitioned to adulthood, I have recently faced my most challenging symptoms. My health is no longer only focused on my bleeding disorder, but also encompasses my bone, reproductive, and mental health due to long time suppression of periods using hormonal therapies. More recently, I suffered a thrombotic event which left me with a portion of permanent blindness in one eye. This experience, as well as my struggles to control my nosebleeds and menstrual bleeding has left me hypervigilant of how being a GT patient affects every aspect of my health.
Although I still struggle with knowing when to get treatment for severe bleeds and don’t have access to prophylaxis treatment, preventative care has still been key in managing my bleeding disorder. This involves minimizing my risks in every activity or environment, and being prepared for every situation.
The bleeding disorders community I have come to know through the World Hemophilia Foundation and the National Bleeding Disorders Foundation (NBDF) in the United States has proved to be an invaluable support and resource. I have met others who have the same bleeding disorder as I have and am inspired to be an advocate for this community <3

I have a child, named Aaron, who was diagnosed with Hemophilia A Severe, when he turned 1 year old in year 2010. He had an episode of intracranial hemorrhage at the age of 2, which almost cost his lives and along the way, had many joint bleeds episodes. At that moment in time, all the hospitals in Sabah, only provided On-Demand therapy.
I was fortunate to be able to communicate and gain knowledge from all the treaters from hospitals and universities, especially the hematologists. In early 2014, I had collaborated with a hematologist from the University Malaysia Sabah to organize a workshop for hemophilia patients in Sabah.
In end of 2014, I was approached by a strong advocate of hemophilia who is also the former President of Hemophilia Society of Malaysia and former Vice President of World Federation of Hemophilia. He encouraged and guide me the way to initiate and set up a Hemophilia Society within my region.
So, in the year 2015, I was involved in advocacy in the form of Hemophilia Society of Malaysia Sabah Chapter because I believe in the power of action to create positive change. Advocacy allows me to use my voice and influence to address issues that matter deeply to me, such as supporting individuals with hemophilia.
By actively participating in advocacy efforts, I can contribute to raise awareness, influencing policies, and fostering a more inclusive and supportive society for those affected by this condition.
Through advocacy in action, I can make a tangible difference in the lives of individuals with hemophilia, helping to ensure they receive the care, understanding, and opportunities they deserve.
I managed to establish a strong network of stakeholders ie.Ministry of Health(Sabah), hospitals(throughout Sabah and Kuala Lumpur), to ensure that the society stays updated with the latest advancements in hemophilia treatment and care. Through strong networking, it facilitates collaboration among the healthcare providers, patients, caregivers, and policy makers. It also increases the society’s ability to access resources.
As a 2024 SSMF Scholarship recipient, I will make the Hemophilia Society stands as a beacon of strength and hope, transforming lives and reshaping the narrative surrounding this challenging condition.
Hola mi nombre es Patricia naranjo y soy mamá de Diego Blankevoort de 7 años quien tiene Hemofilia A severa soy portadora de hemofilia mi padre tenía hemofilia y cuando nació mi hijo nunca imaginé que el podría tener y así fue desde un año que Diego usa la profilaxis el se inyecta hoy en día 1000 de liofilizado y nos a echo la vida más fácil y para mí niño la vida normal estoy muy feliz por su tratamiento ya que si el Diego se pone mal nunca debe de faltar a su tratamiento siempre al pie de la letra vamos hoy en día yo aprendí a inyectarlo gracias al centro de hemofilia del Hospital Roberto del Río y asus profesionales en especial ala doctora Verónica Soto la mejor doctora que le tocó a mi hijo y así vamos viviendo día a día su enfermedad se puede vivir en armonía y tranquilidad.
I am a mom of four beautiful children, with one having moderate Hemophilia A (however, he bleeds as a severe). He is my second youngest and most defiantly the most wild out of my bunch. From 7.5 years ago, when we found out Elias has hemophilia shortly after birth, life has has it challenges but most importantly its brought us into an amazing community that I cannot be grateful to be apart of.
When Elias was first born, we knew pretty soon after birth, that something was not right. He bled, and bled, and bled for days. We later were finally transferred to Vanderbilt Children’s Hospital where we found that he had Hemophilia A. What a day that really was. From being exhausted from having a new baby, to finding out that he has a serious condition, it really took a toll on me, as his mom. From that day though, I knew that I had to become Elias’ expert of his body and his condition because I was not only a mom now, but his advocate as well.
Early on, things were okay and we treated as needed. He started walking, and we had to have a few infusions from him falling and bruising that just would not stop growing. He started talking, and we had multiple infusions from mouth bleeds from him biting his tongue. When he was 2, we spent Christmas Eve in the hospital from an ankle bleed that we assume he got from walking on gravel (but who really knows). A few months later he got another joint bleed but this time in his elbow that we concluded had to of been spontaneous. At this point, I knew I had to stand up for him and decided that we needed to start on prophy because I could not deal with my son being in so many pain and treating afterward. After much fighting with insurance, he was finally approved to start emicizumab.
Emicizumab has absolutely been life changing for us. While I had never limited Elias from doing fun boy things, like riding his bike, jumping on a trampoline, doing backflips off the couch, riding a dirt bike, you know all the “fun” things that kids like to do, emicizumab sorta gave a peace of mind as well. Literally 3 months after his elbow bleed, he ended up breaking his other arm while in a bouncy house, ONLY MY CHILD RIGHT? LOL. We infused as a precaution but I really believe that because he has emicizumab, his injury was not worse.
Elias is now 7.5 and is NOT a poster child of Hemophilia. I let him do all the fun things that he wants to do (for the most part anyways). I fully believe that if I do not let him learn his own limitations now and let him “live in a bubble” then things will only get worst as he gets older. He plays baseball and is aggressive in his position and I think its great! He does not let Hemophilia define his life and I don’t either. Our life may be a little different from others, we may have to do things a little differently, but as a mom of hemo hero, my mind now thinks differently too.
We have started bringing awareness to our local community as well as bringing it all the way to Washington D.C. Nobody knows if they simple just don’t know. It is our job to bring attention to the matter and bring the awareness because I too, was one of those who had no idea that the word “hemophilia” meant. I love this journey that we as a family are now embarking. Elias is learning to advocate for himself, his siblings are also aware and are able to bring awareness to who around them too. Hemophilia not only affects the one who has it, but the entire family as a whole. We must support, advocate, and deal with it together to come out stronger and better than ever. Hemophilia will never stop Elias, it just may try to slow him down, but we are there to support and push him, because it will never win; we will not let it!

Dear All,
My name is Phyo Khant Kyaw, and I am writing to share my journey as a severe Hemophiliac with Factor-IX deficiency from Myanmar.
In 1998, I was faced with the harsh reality of my condition when a simple injury to my gum led to a diagnosis that changed my life forever. At that time, diagnosing Factor deficiency in Myanmar was a challenge, and I had been on a journey over thousand blood transfusions.
Despite the countless transfusions, my knowledge of hemophilia remained limited. When I became a member of the Myanmar Hemophilia Patient Association (MHPA), I was able to connect with others facing similar challenges, and together, we shared knowledge, experiences, and support that empowered me to navigate my condition with greater confidence and understanding.
One of the most harrowing moments of my journey was experiencing an intracranial hemorrhage during my childhood. I was engulfed by fear, unable to speak, and unable to see the light . However, care and treatment provided by Pf. Aye Aye Khaing, I got recovery within two weeks.
Until 2016, the absence of Factor-IX treatment left, resulting in deformities in both knees and my left elbow. However, in 2017, with the introduction of Factor treatment, a new chapter of hope began.
I am immensely grateful to the World Federation of Hemophilia (WFH), whose saving my life and the lives of countless others affected by this condition. Through their initiatives and advocacy, individuals like myself have been given a chance at life, hope, and a brighter future.
In closing, I extend my deepest gratitude to Pf. Aye Aye Khaing, the Myanmar Hemophilia Patient Association (MHPA), and the World Federation of Hemophilia (WFH).
With heartfelt appreciation,
Phyo Khant Kyaw

Terapeuta Hemato-Onco formada para peques con Hemofilia sin conocer que la vida me preparaba para atender a mi propia familia. Oaxaca-México
This is my Journey of living with Haemophilia.
When i was 11-year-old, there was great debate regarding my circumcision among the family. Elder members like my grandmother and uncles, remembering the death of my uncle due to non-stop bleeding, resulting from the circumcision as per the Muslim tradition in Sudan. My father, one of the admirers of Dr. Faroog Sidiqu, the reputed hematologist at the Khartoum Hospital, suggested that it is the doctor who would decide on it. My father was right. He could remember, the son was laying on the bed at that regional hospital, between life and death, bleeding for the third consecutive day. Doctors were puzzled and almost exhausted all options to stop this nasty bleeding from the nose. He took the journey from, after losing hopes, from Berber to Khartoum, not quite sure that his beloved son would make it. Dr. Faroog was in charge of the case. The child was admitted in the hospital, blood transfusions were made one bottle after another, and many tests were done.
– your son is confirmed to have a bleeding disorder, do you have any similar issues in the family? Asked Dr. faroog
-Yes, two of his uncles, mother’s brothers died at age of 9 and 13. Father replied.
-He is lucky to be born in an era that witnessed many improvements in the medical care of this clotting problem.
I was admitted at Khartoum Hospital for almost a week with the plasma infusion undertaken every 12 hours. the doctor assured there is a new medicine which would be a game changer in the lives of poor hemophiliacs. that was almost in 1971 when i was diagnosed and had my first treatment. My father and I came back to our home in the town of Berber, 360 Km north of the capital overwhelmed by the cheers of the relatives who presumed a miracle has been taking place and overloaded with many advice of the doctor on how to handle the case of boy. From that day i became a regular visitor to blood bank of Kh Hospital.
I went to the toilet, secretly wished to evaluate the efficiency of this medicine by myself. i was admitted because there was blood in my urine that lasted for couple of days. I came our rushing to my father, ” Yes, it is working dad, oh my God”.
What is working? asked my dad?
“The medicine” .i replied back………. “My urine turned to light yellow instead of red.”
it was a simple verification of the worthiness of the injected medicine. Color is changing from red to light yellow. i was stunned. my doubts turned into firm belief.
1976, i completed 10 years, with many self-awareness about the line that has been drawn. i sensed the attention of many eyes focusing on anything that i was doing. Playing football with my peers was a big taboo. I loved football and exhibited remarkable skills in playing. yet my friend would be very reluctant to let me play with them. They are afraid of the subsequences. At school the story was a bit different. The teachers were well informed about my case and warned that any physical punishment my lead to serious subsequences. I was very good at all subjects and topped the class. Not giving any teacher any reason to push me. Lashing the boys with whips was a common practice and the teachers were authorized to do it. when there a common punishment, the teacher would exclude me. some would make their own punishment for this strange boy. Mr. Amin, our math teacher, looked at me from face to toe and mockingly asked the class to stand up. it happened that i came late that morning and he was already in the classroom. He instructed the students to Welcome “His Highness” by singing the National Anthem. They did. He was so cruel to vent his anger in that way. i was down morally.
The same year, in the school holiday, my dad and i travelled to the capital by Half Express train. It was a privilege to travel to Khartoum, envied by my friends and give me times to narrate the wonders i have seen in Khartoum. They do not know that if it were not for this bleeding issues i would have never visited the capital. My wonder was that i had nothing this time to explain why we had to go to the capital. my health was great and no bleeding, being inside or outside.
The discussion was going on that morning with Dr. Faroog and some other big consultants providing more assurances to my dad that circumcision like any surgery would be efferently managed by the administration of the factor, factor 8.
Although i was cent per cent fit, i was admitted at the Pediatrics Section at the Hospital. Factor replacement was planned twice a day. My dad, noting the growing frustration inside me for being injected without a valid reason, he told me we planned to circumcise you. it is a simple procedure and there are no worries. I was a bit relived. Circumcision is something that relates to manhood in that closed environment. A man uncircumcised is not a man.
The day came. The news spread everywhere and our far and near relatives came to witness this “operation”. some of them, had no trust in the medicine at all, objecting seriously and surrendered to the will of my father who swear would never leave his son uncircumcised whatsoever. Three of the surgeons attended the surgery. Dr. Faroog set the hemostatic management plan with close monitoring of all essential parameters. After an hour i was pushed on a wheeled chair to the room. My aunts and other women ululated in joy. i spent around two weeks under the persistence of the medical team who left nothing for the chance. i was under the factor coverage for the entire period. Very minimal bleeding was observed. We returned to our hometown like a victorious army. when the train stopped at the station, we found a fleet of around 4 cars awaiting us. Celebration had to start and many cow blood were shed and many people were coming in to see the wonders, especially elders whom the occasion evoked their bitter memories of the earlier death of my two uncles.

JOURNEY WITH HEMOPHILIA
I am T. Jaipal, 73 years old ,Member and Treasurer of Hemophilia society Pondicherry chapter. My journey remained from South to North and North to South .
I was born on 6thOctober 1950 at Chennai. My father being central government staff got transferred to Jabalpur and we got settled there. Up to 12 years of my age days passed with full of pain and treated with Home remedies. There was a small Rt knee hit and from then onwards spontaneous bleeding occurred with a big swelling and intolerable pain. In spite of pain killer medicine taken, Rt, Knee got totally stiff and then onwards RT Knee had contracture. Then many episodes of joint and muscle bleed occurred, and I started my career along with the pain and Courage given by God .
I completed my HSSC examination and joined Central Government as LDC Staff. From then onwards I reached up to Office Superintendent Level -1, in Administration Division, in no time I became handicapped due to repeated joint and muscle bleed
Things were going normal and one fine morning spontaneous Gum bleeding occurred and it took 3 to 4 days to become normal. In the year 2004, September Intra Abdominal bleed occurred and not able to find reason and 10bottles of wholesome blood given to stop the bleeding. I again consulted with the Dr’s and again Medical checkups was done thoroughly and found that it is blood clotting disorder Hemophilia. Blood Assay was done and found F VIII < 1% which is severe. Then I got Registered in Hemophilia society Jabalpur as a member.
In the month of April 2006 I got Voluntary Retirement leaving 5 years service. I had an opportunity to settle in Pondicherry along with my son and my wife. Since 2011, we settled in Pondicherry. I called Mr. A. Balaji, secretary of Hemophilia society Pondicherry chapter,and he advised me to contact Dr. P. Nalini, and get registered in Hemophilia society Pondicherry chapter. Then Dr. P.Nalini called me over phone to come to office immediately and she examined all the medical records and told to get registered in the Pondicherry chapter. She felt very sad due to disability happened to me
From then onwards Dr. P. Nalini is fully taking care of me. She with the help JIPMER Central Government Health Scheme, received Factor VIII for me as regular prophylaxis. It would not be out of order to say that Prof. Dr. P. Nalini is GOD for Hemophiliacs of Pondicherry chapter providing personnel touch to all hemophiliacs irrespect of caste, creed and colour. This year 2023 Prof. Dr. P. Nalini is awarded with Padma Shri by the Government of India.
I am living peaceful life with the help of Hemophilia society Pondicherry chapter,
JIPMER Doctors, Central Government Health Scheme, and along with my family support also.
Thanking you,
Treasurer and Member
Hemophilia society Pondicherry chapter

Hi, Greetings for the Day.
I myself Mr. Pritish Navnath Desai sharing a story whether its success story or struggle story that you all decide. The guy name Pritish born on 14 October 1985 as a healthy and active baby. All three families Desai Family, Mhatre Family , Pathare Family were into celebration. Their celebration won’t last for long as when I was 1.5 year old I diagnoses with Haemophilia B factor 9 deficiency less than 1 ℅ . All three families are in tense but DIN of Wadia Hospital Dr. Karim Boy and their team help me to meet my success. I have seen lots of bleeds, many times I given the exam from hospital. So many things. I have seen many downs in my life specially love life due to Haemophilia , but it was ok. I have Lost opportunity to join Indian Air Force, also Lost precious job in Icici Bank due to this, but it was ok. But one Company stands with me that’s Jaguar LandRover it helps me grow it teaches me engineering skill, although I am MBA in finance and MBA in banking.
When I look back I See the guy who destroy thousand times and rebuilt. That’s me.
14/6/1994 a day after joining as Paediatrician in Government Hospital Aluva. Called to see a boy with excruciating pain and swelling of the knee joint, I was totally at a loss as to how to manage the case. The patient had a white ID card from Christian Medical College, Vellore identifying him as Hemophilia A severe patient. I rushed to my adjacent RMO Quarters to check with Nelson’s Text Book of Paediatrics as I had not seen a case of hemophilia before. The only option at that time was Cryoprecipitate which was available with the Components Separation Unit at Cochin. With 6 units twice daily he became alright. The child’s younger brother had added Duchenne Muscular Dystrophy also an X-linked disorder that proved fatal and he succumbed to respiratory paralysis below ten years of age.
Brush with this thereto unfamiliar disease made me associate with HFI (Haemophilia Federation of India) Ankamali chapter. At their request, we arranged a component separation license to ensure a free supply of cryoprecipitate the only treatment available. Occasionally the Chapter used to receive factor concentrates from the World Federation of Haemophilia as donations. However, the patient conclave organized in 2012 with the participation of local bodies and ministers proved to be an eye-opener and on World Hemophilia Day 2013 the foundation stone for the first and only Comprehensive Haemophilia Treatment Centre was laid. On February 20th, 2014 the Centre was opened by the Chief Minister who announced on-demand factor treatment for children below 18 and a monthly pension of Rs.1000/- The very next year 20th March 2015 at the valedictory function of the National HTC conclave hosted by us the Chief Minister announced the extension of ODT to all patients and prophylaxis for children in the District. In 2021 the Government of Kerala under the Asadhara programme extended Universal Paediatric Prophylaxis and adult ODT in the state. In 2020 we started nonfactor therapy also and now we have ten kids on Emicizumab. We could contribute in our own humble manner to the advocacy efforts along with HFI. My 50 years long stint with Health Services Department was also helpful. We are helped by the Hematology Department of Amrita Institute of Medical Sciences.
We have 1071 PwH enrolled here (883 HA + 188HB) Looking back on the plight of PwH. Our laboratory has EQADS with WFH and Christian Medical College, Vellore. The centre is a participant of WBDR and just completed 4 years WFHTwinning Programme with New Castle upon Tyne. We have had 24 publications in the last 9 years. WFH recognized our WBDR performance, Twinning efforts, and Laboratory services.

Sufro de von willebrand, ya que la heredé de mi papá. Soy la tercera generación con esta condición, siempre pensé que era normal tener anemia y sangrados abundantes durante mi menstruación (igual que mis tias), pero al salir del país me di cuenta que hay otras opciones para las personas con mi condición y que no tenía que vivir con anemia, así que gracias a la hematologa que me atendió en Ecuador empecé a tomar acido tranexanico y desmopresina, eso me ayudó bastante y pide tener un mejor control del sangrado. Actualmente uso Mirena y la menstruación prácticamente se detuvo. También solo uso factor cuando tengo una operación o extracción dental, y por primera vez tengo factor en casos de emergencia, por lo cual estoy muy agradecida, ya que hace un par de años tuve una operación y durante el postoperatorio tuve una hemorragia y nada de factor para poder controlarla. Solo el ácido tranexanico me ayudó en ese momento. En fin, agradezco a todos los que me han ayudado en este camino de padecer von willebrand y que me enseñaron que se puede tener buena calidad de vida a pesar de los sangrados.

Hola me llamo Nayeli Dueñas soy mamá de Ian Lozano un pequeño de 6 años con Hemofilia A Leve , a Ian le detectaron la enfermedad cuando el tenia apenas 2 añitos en mi experiencia puedo decirles que siendo una enfermedad tan rara y muy poco conocida me inundó y nos inundó a mí , a mi esposo y a mis hijos un miedo terrible y más por qué veíamos a ni ñino tan chiquito y tan indefenso …
Hoy gracias a su tratamiento , a la información que se brinda acerca de la Hemofilia, a los especialistas que llevan su caso y a mi familia por el apoyo hoy mi hijo lleva una calidad de vida mejor y esperemos que así siga …
Un beso y un abrazo desde Guadalajara Jalisco México !

Hola me llamo Casandra Ramirez y soy madre de un hijo hemofilico ,se llama Juan Antonio de 16 años, el cual tiene 2 hermanas mayores podrán imaginarse que Juan siendo un hombresito después de 2 mujeres ,me sentía realizada como madre ya mi hijo varón y fue 6 meses después de su nacimiento que descubrimos que era hemofilico , en esos momentos mi mundo se vino abajo ,solo pensaba que mi hijo moriría en cualquier momento ,no teníamos nada de conocimiento referente a la enfermedad ,ni medicamento ,…fue tan doloroso ver Ami hijo llorando por las noches con tanto dolor en sus tobillos por el simple hecho de querer llevar una vida como cualquier niño de su edad..pero gracias a Dios a la edad de 6 años buscamos ayuda en otro estado ,llegamos a nuevo león directo al hospital universitario buscando atención para mi Juan y así fue me dijeron que podía llevar su tratamiento y atención personalizada con hematólogo,trauma,genética…y fue ahí donde aprendimos a tratar la hemofilia cómo un padecimiento llevadero con sus cuidados y profilaxis pertinente ,agradezco enorme mente a la Dra. Villarreal encargada de la clínica de hemofilia y la Lic. Laura Páez nuestra trabajadora social que siempre nos llevan de la mano cada una en atención física y atención emocional ya que la Lic. Laura Paez siempre está al pendiente de que nosotros como padres seamos responsables y puntuales con esta atención para nuestros hijos …desde que llegamos a la clinica de hemofilia del hospital universitario nuestra perspectiva de vida cambio ,hoy por hoy se que mi hijo puede realizarse como cualquier otro adolescente y todo es por educarnos respecto ala hemofilia y claro llevar su profilaxis correctamente ..nunca perdamos las esperanzas …gracias
Hola buen día
Solo paso por aquí a saludar y a contar
Soy portadora Hemofilia Severa
Tengo un hermano vivo Hemofílico y uno ya fallecido
Dos primos vivos

أطيب التمنيات باليوم العالمي للهيموفيليا انضممت إلى الاتحاد العالمي للهيموفيليا في عام 2015 – في البداية كمدير إقليمي لإفريقيا والشرق الأوسط والآن أغطي الشرق الأوسط فقط. كانت السنوات الثماني الماضية رحلة رائعة للقاء العديد من الأشخاص الملهمين المصابين بالهيموفيليا والأمهات والآباء والإخوة والأخوات ولقاء الأشخاص في المجال الطبي المهني الذين يعتنون بهم والحكومات التي تدعمهم. من خلال هذه الرحلة ، تعلمت أنه من خلال الجهود التعاونية لجميع أصحاب المصلحة ، يصبح حتى الهدف الأكثر صعوبة أو بعيدًا ممكنًا. إن الجهود الدؤوبة لهذا المجتمع هي التي ستستمر في تحقيق اختراقات في توفير الوصول إلى العلاج لمن هم في أمس الحاجة إليه. استمروا في العمل العظيم. إنه لشرف لنا أن نلتقي بكم جميعًا ، ، وأن نقرأ قصصكم الجماعية وأن نعمل عن كثب مع العديد منكم وندعمكم بأفضل ما نستطيع
I wanted to share a really nice experience I had recently with one of our adolescent females, with Von willebrand disease, who has moved from children’s services to our adults.
She had seen our consultant in clinic & arranged to come & learn how to self inject DDAVP for period management, alongside starting tranexamic acid.
Asides from making me feel old because I remember her being born, her dad has Von willebrand disease and we look after multiple generations of her family, it was really great to spend some quality time with her going over her disease, access to care & teaching her how to treat.
About 10 days later she made contact and asked to come back and run through some bits. I thought perhaps I’d missed something with her self administration education but on arrival she produced a list of questions for me.
We proceeded to spend 45-60 minutes going through more details about treatment options, including an introduction to treating with Von willebrand factor concentrate if DDAVP did not prove adequate for bleeding control. We discussed how & when she can access treatment, other options for period management including the option for joint review in our gynaecology/bleeding disorders clinic, supporting her in university choices, holiday advice & general day to day advice & discussion about her condition.
Unfortunately this young lady fell victim to nearing adult transition during the COVID pandemic and therefore didn’t get the same options of regular joint appointments. Luckily with her family knowing the adult team well she felt comfortable coming in & discussing her options for access care & treatment.
At the end of the day, this is why I love the job I do, because these two conversations have been beneficial to the affected Individual & their parent in providing reassurance about their next steps in life & that we have other treatment options available. I was also able to let her know that the bleeding she was experiencing isn’t normal & we can help to resolve that as well as provide iron supplements to support blood loss until bleeding settles.

My Brain surgery with the help of Afstylia Factor support from WFH
Sankar@ Sanakaranarayanan
I am Sankar@ Sanakaranarayanan from Tindivanam, South India hails for lower socio economic group. In my child hood I was taken to various Hospitals for various treatments for my various bleeds and nobody diagnosed me as Hemophilia. I suffered many bleeds like oral bleeds, joint bleeds and muscle bleeds,and I, and at the age of 7 only I am diagnosed as Hemophilia A. I have 1 elder sister and 4 younger sisters and my 3 nephews are affected by Hemophilia A . Before 25 years there was no factor and all the way Plasma was transfused and it was given for all treatment and surgeries also. Later I found that there was a registered society in Madras for Hemophilia. So I and my 3 nephews registered in Madras society and we went for treatment in Madras Society.
Some years later I heard that Dr. P. Nalini, Professor of Pediatrics, JIPMER, Pondicherry (Retd) had started Hemophilia society Pondicherry chapter and I submitted all the documents of myself to Dr. P. Nalini and I became a Life Member of the Pondicherry Hemophilia society. I underwent 2 major surgeries and with the help of Factor from Hemophilia Federation India, New Delhi and also support given by Dr.P. Nalini, which are all Free of Cost. In the year 2018, I had severe fever and I came to JIPMER and there I was diagnosed as Malaria and due to Malaria I had blood clot in my brain and the clot was diagonised by Neuro Surgeon of JIPMER and open surgery was done in JIPMER, which was also Free of Cost , and full Factor support(Afstylia) was given by Hemophilia society Pondicherry chapter obtained from World Federation of Hemophilia, through Hemophilia Federation (India). After my surgery I was supported by Factor for 6 months as prophylaxis and I am fully recovered. In spite of various bleeds and I am fully recovered from IC Bleed ,and I am now normal. My family members express their gratitude to WFH , HFI (India) an Hemophilia society Pondicherry chapter
Thanks to all
E. Sankaranarayanan
M. NO. 53
Hemophilia society Pondicherry chapter
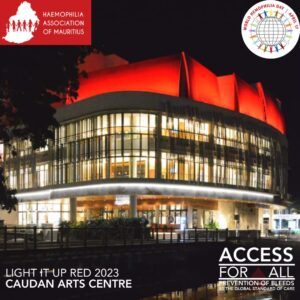
The Haemophilia Association of Mauritius wish you all a Happy World Haemophilia Day 2023. Access for all. Cheers to all our Heroes.
Rajesh Neelayya
President
Haemophilia Association of Mauritius.
As hemophilia caregiver , many positive stories are with me, but most exciting ones are : life of one child with brain Hemorrhage is saved with continuous and untiring efforts of his mother and now that child has normal actovity without any residual disabilty , it is really most satisfying event in my life as hemophilia physician and other adult patient came to my care when there was plan to have amputation of the leg and with personal care leg is saved .That boy had nailing a d plating for fracture without factor support
Здравствуйте, уважаемые сотрудники WFH!
Узнав о том, что скоро будет Всемирный день гемофилии, решила написать вам благодарственное письмо. Вот уже более 50 лет вы сосредоточены на помощи и спасении больных. И сегодня, благодаря вашей деятельности, диагноз “гемофилия” перестал быть смертным приговором. Спасибо вам огромное за то, что посвятили этому свою жизнь!
Скоро христиане будут праздновать Пасху. Всем известно, что Иисус Христос воскрес из мёртвых. Однако, не все знают почему Он умер. На этот вопрос исчерпывающе отвечает Священное Писание: “Бог любит мир так сильно, что отдал своего единородного Сына, чтобы каждый, кто в него верит, не погиб, а обрёл вечную жизнь” (Евангелие Иоанна 3 глава, 16 стих). Из любви к людям Бог отдал своего дорогого Сына в жертву, а Иисус, в свою очередь, согласился принять мученическую смерть ради того, чтобы избавить человечество от греха и смерти, который мы унаследовали от первой человеческой пары. Грех можно сравнить с генетическим заболеванием, которое передаётся от родителей к детям. Христос, своей жертвенной смертью, открыл перед человечеством возможность жить без этого угнетающего “заболевания”. Вскоре послушные Богу люди смогут жить вечно, без боли, страданий и даже смерти.
Спасибо ещё раз за ваш ценный труд!
Желаю успехов в труде, и крепкого здоровья вам и вашим близким.
С уважением, Наталья.
Hello all,
As the editor of the WFH News page, I’m always covering the latest news in hemophilia, and sharing the latest developments for people with bleeding disorders. It’s a rewarding job, but the most interesting day of the year for me is World Hemophilia Day, because that’s when I get to read heartfelt stories shared by people from around the world. It’s really inspirational to read about your courage, and your strength! Keep it up. I look forward to hearing more from you, as I know the the other people in our community do.
Mitch
Editor, WFH News

I am a severe hemophiliac with factor-VIII deficiency. I am from a remote island district of Bangladesh. I passed my early life without any treatment but to use ice available in fishing village near our village home. Yes I had a very critical life during my school life still I was able to complete my school education with good grades and able to get admission into Dhaka University, which actually changed my life’s goals. Then I got to be able to get in touch with WFH and Mr. Ashok Verma, the founder of HFI. He guided me to establish Hemophilia Society of Bangladesh.
And I have been working with HSB for last 28 years. It’s my pleasure to be a part of great transformation of HSB to new dimensions and the changing approach of government towards hemophiliacs is a great achievement of my life. We are now getting some factor support from government.
I am an avid solo traveler and enjoy my vacation days around the country, sometimes outside country. My physical disability cannot stop me to go around and enjoy my life. Yes I am fond of adventure traveling, whatever my body permits. I love my life, I love hemophilia, it infact strengthen my life.

Celebrating World Haemophilia Day 2022
If you have not seen or heard of heroine’s, here is one that inspires my work. Ba Egrain Ngandu from Kasamba village, Chief Hanjalika, Mazabuka District, Southern Province.
The woman you see in the two picture with her husband gave birth to 18 children of which 9 died because of haemophilia.
Trust their last son living with the condition is a clear testimony of how donated products by the World Federation of Hemophilia WHF have transformed the lives of the people living with haemophilia in Zambia.
I am greatly inspired.
Happy World Haemophilia Day to the bleeding disorders community around the Globe.
I have Severe Hemophilia A and have suffered from many complications from it. The continued support of organizations that help people suffering from this debilitating disease and all the help from supporting friends, family and colleagues has allowed me to live a relatively great life. Hoping the best for everyone who is suffering from Hemophilia. Goodluck!

I am a patient with HEMOPHILIA, I was diagnosed at the age of 10 months. Later I was found Sero Positive in 1996. I was the first patient of The Haemophilia Society Calcutta Chapter who started Anti Retroviral Therapy. This year my DIALYSIS HAS STARTED SINCE JANUARY 2022 as my kidney stopped to work. Again I am the first patient of the Haemophilia Society Calcutta Chapter who is on PERITONEAL DIALYSIS which is too expensive for me.
The H.T.C. of Calcutta Chapter has helped me a lot in my crisis period. I am thankful to the Haemophilia society Calcutta Chapter, Hemophilia Federation India, World Federation of Hemophilia.

I’m Syed Shabistan, a severe Hemophilia A from Peshawar, Pakistan.
I’m the part of spreading the WFH awareness campaign about bleeding disorders all over the globe & especially want to aware & facilitate my own community members of Hemophilia Patients Welfare Society Peshawar, Pakistan
اسمي رنا الصيفي وانا مسؤولة الشرق الاوسط في الاتحاد العالمي للهيموفيليا منذ عام ٢٠١٥.
الاحتفالات الرائعة باليوم العالمي للهيموفيليا في جميع أنحاء العالم وخاصة في منطقتنا العربية مدعاة للفخر والسرور معا. لدينا منظمات وأعضاء مجتمع افراد نزف ملتزمون بشدة، ومبدعون ونابضون بالحيوية في معظم دول الشرق الأوسط (آمل أن يجد أولئك الذين يكافحون مصدر إلهام للحاق بأقرانهم في اسرع وقت ممكن). إنكم تثبتون لنا يومًا بعد يوم ، مدي شجاعتكم وباسكم والتزامكم في الدفاع عن حق الجميع للحصول علي العلاج بشكل أفضل. أرق التحية وخالص الشكر النابع من صميم القلب لكافة مجهوداتكم اليوم وكل يوم. كل عام وانتم جميعا بخير. استمروا في التألق الأصدقاء والزملاء الأعزاء
My name is Tai-il Kim.
I have severe hemophilia A. And I have two sons and a youngest daughter. The daughter is 4 years old and of course a hemA carrier. I usually ask my children to help me when I self-inject to inform them about hemophilia in a friendly way.
Yesterday, I had a prophylaxis with my daughter. For the first time, she succeeded in stabbing the needle, even though I held her hand.
By the time our children grow up and give birth to their children, they’ll have completely overcome their hemophilia, and they won’t get these injections anymore, right?
Today, April 17th, World Hemophilia Day, I wish better treatment for hemophilia and better awareness of more bleeding disorders.
https://youtu.be/HLnTYmFc-aM

I have Von Willebrand’s disease. The diagnosis was made only 4 years ago. Now I am receiving preventive treatment. It’s scary to remember what happened before this treatment. This disease has severely undermined my health

My name is Atharv Pareek, I have Severe hemophilia A type disease, due to this disease I am not able to go to school properly nor play with friends, I have to go to the hospital 3 days a week to take the factor VIII. By taking the reason of the factor, my joints are still fine, I have thanks to the Government of Rajasthan and the World Haemophilia Federation, due to which I get these medicines free of cost. If such a medicine is made, which is to be given only once a week, then how much relief will it be for me?
Thanks 🙏🙏🙏
Yes, my story is no difference between it and most of the stories of hemophilia patients at the beginning of my life and at the age of eight months, my mother discovered that I had hemophilia through blue spots on my body as well as bruises. Examination, diagnosis, and providing treatment for me was like a horror movie for my parents, as they knew the disease from before I was born and my son was dedicated to my safety. In my childhood there was a kind of follow-up and control in terms of what games and sports were allowed and not allowed. I was wondering at the beginning of my life why my mother not Do you promise to run and play with the rest of the kids? When I joined a school, it was normal for me, but for my family, it was stressful and tiring (knowing that I have siblings who are sick with the same disease). The aim of this is to make my identity known to all my colleagues, as well as the staff and school workers. I was very happy because everyone knew me and very sad because I could not play with my colleagues. The teacher did not leave me for fear and for my safety. I was very upset. I entered the department first and came out last. And the teacher held my hand until she handed me over to my mother or older sister in order to take me home in the evening at the end of work. I would secretly go outside to meet with my friends to play football, but they would not leave me or invite me because my mother and father had betrayed them from my playing football The foot is the reason that it causes me harm, so I begged them to play just a little bit, so they let me play and pass the ball to me and let me dribble and run without anyone in the way, then we think about football to play hide and seek and several traditional games and in the evening when I come home, my mother tells me no One day you will bleed and you will scold me and keep me at home so that I can go back to my lessons, and then the joint pain starts, especially the knees and ankles. I go to my mother and tell her that I am not okay, so she reprimands me and takes me to the hospital every time … a medical examination, a diagnosis, I take a dose of Factor 8 and go home And my parents are loaded with medicines and I have a needle implanted in my elbows… Relax and then resume playing electronic games and dominoes and read books and review the lessons that I missed under the supervision of my little teacher (my older sister) and my father. Especially at night and I was encouraging myself that nothing would happen to me and I would not repeat mistakes and I would study hard in order to excel and be the happiest of those who worked for me…. Mom and Dad always tell me that you are the reason for what happens to you and that you are a child you put yourself in trouble and Problems because you are not convinced that you are not like other children, my father talks and says that if you do this again, you will not go for a picnic, and I will not buy you what you want, and I will punish without hitting you, I will deprive you of all the things you want, so ask their forgiveness and I will not repeat this and I will I obey them and take care of myself knowing my mother is a nurse and she was always keen on my safety at home At school and outside, she alerts my friends and advises them about my safety. At home, my brothers gather and tell them to be careful of his safety in my absence, me and your father. Do not let him leave the house. Do not create problems with him. If he insists on leaving, call me or your father… .. Such are the sacrifices that parents make for the sake of their children …. I was a son who caused trouble and my daughter used to advise me and teach me the meaning of hemophilia patients and its types and what are its symptoms and dangers, and she encouraged me to practice swimming until I became proficient in it … She taught me how to inject Myself used to give me health education lessons, and my father used to take me daily to school in the morning and come back in the evening to take their advice. I realized it at the age of fifteen when I entered high school. Today, I am a young man, enjoying good health, and following my preventive treatment, thank God, knowing that my knee joints are very affected. Because of inflammation, but thank God I can move and help others, knowing that I am an association founder in my state and a contributor to providing a helping hand to hemophilia patients. Thank you
I am a mom of four beautiful children, with one having moderate Hemophilia A (however, he bleeds as a severe). He is my second youngest and most defiantly the most wild out of my bunch. From 7.5 years ago, when we found out Elias has hemophilia shortly after birth, life has has it challenges but most importantly its brought us into an amazing community that I cannot be grateful to be apart of.
When Elias was first born, we knew pretty soon after birth, that something was not right. He bled, and bled, and bled for days. We later were finally transferred to Vanderbilt Children’s Hospital where we found that he had Hemophilia A. What a day that really was. From being exhausted from having a new baby, to finding out that he has a serious condition, it really took a toll on me, as his mom. From that day though, I knew that I had to become Elias’ expert of his body and his condition because I was not only a mom now, but his advocate as well.
Early on, things were okay and we treated as needed. He started walking, and we had to have a few infusions from him falling and bruising that just would not stop growing. He started talking, and we had multiple infusions from mouth bleeds from him biting his tongue. When he was 2, we spent Christmas Eve in the hospital from an ankle bleed that we assume he got from walking on gravel (but who really knows). A few months later he got another joint bleed but this time in his elbow that we concluded had to of been spontaneous. At this point, I knew I had to stand up for him and decided that we needed to start on prophy because I could not deal with my son being in so many pain and treating afterward. After much fighting with insurance, he was finally approved to start emicizumab.
Emicizumab has absolutely been life changing for us. While I had never limited Elias from doing fun boy things, like riding his bike, jumping on a trampoline, doing backflips off the couch, riding a dirt bike, you know all the “fun” things that kids like to do, emicizumab sorta gave a peace of mind as well. Literally 3 months after his elbow bleed, he ended up breaking his other arm while in a bouncy house, ONLY MY CHILD RIGHT? LOL. We infused as a precaution but I really believe that because he has emicizumab, his injury was not worse.
Elias is now 7.5 and is NOT a poster child of Hemophilia. I let him do all the fun things that he wants to do (for the most part anyways). I fully believe that if I do not let him learn his own limitations now and let him “live in a bubble” then things will only get worst as he gets older. He plays baseball and is aggressive in his position and I think its great! He does not let Hemophilia define his life and I don’t either. Our life may be a little different from others, we may have to do things a little differently, but as a mom of hemo hero, my mind now thinks differently too.
We have started bringing awareness to our local community as well as bringing it all the way to Washington D.C. Nobody knows if they simple just don’t know. It is our job to bring attention to the matter and bring the awareness because I too, was one of those who had no idea that the word “hemophilia” meant. I love this journey that we as a family are now embarking. Elias is learning to advocate for himself, his siblings are also aware and are able to bring awareness to who around them too. Hemophilia not only affects the one who has it, but the entire family as a whole. We must support, advocate, and deal with it together to come out stronger and better than ever. Hemophilia will never stop Elias, it just may try to slow him down, but we are there to support and push him, because it will never win; we will not let it!

Dear All,
My name is Phyo Khant Kyaw, and I am writing to share my journey as a severe Hemophiliac with Factor-IX deficiency from Myanmar.
In 1998, I was faced with the harsh reality of my condition when a simple injury to my gum led to a diagnosis that changed my life forever. At that time, diagnosing Factor deficiency in Myanmar was a challenge, and I had been on a journey over thousand blood transfusions.
Despite the countless transfusions, my knowledge of hemophilia remained limited. When I became a member of the Myanmar Hemophilia Patient Association (MHPA), I was able to connect with others facing similar challenges, and together, we shared knowledge, experiences, and support that empowered me to navigate my condition with greater confidence and understanding.
One of the most harrowing moments of my journey was experiencing an intracranial hemorrhage during my childhood. I was engulfed by fear, unable to speak, and unable to see the light . However, care and treatment provided by Pf. Aye Aye Khaing, I got recovery within two weeks.
Until 2016, the absence of Factor-IX treatment left, resulting in deformities in both knees and my left elbow. However, in 2017, with the introduction of Factor treatment, a new chapter of hope began.
I am immensely grateful to the World Federation of Hemophilia (WFH), whose saving my life and the lives of countless others affected by this condition. Through their initiatives and advocacy, individuals like myself have been given a chance at life, hope, and a brighter future.
In closing, I extend my deepest gratitude to Pf. Aye Aye Khaing, the Myanmar Hemophilia Patient Association (MHPA), and the World Federation of Hemophilia (WFH).
With heartfelt appreciation,
Phyo Khant Kyaw

Terapeuta Hemato-Onco formada para peques con Hemofilia sin conocer que la vida me preparaba para atender a mi propia familia. Oaxaca-México
This is my Journey of living with Haemophilia.
When i was 11-year-old, there was great debate regarding my circumcision among the family. Elder members like my grandmother and uncles, remembering the death of my uncle due to non-stop bleeding, resulting from the circumcision as per the Muslim tradition in Sudan. My father, one of the admirers of Dr. Faroog Sidiqu, the reputed hematologist at the Khartoum Hospital, suggested that it is the doctor who would decide on it. My father was right. He could remember, the son was laying on the bed at that regional hospital, between life and death, bleeding for the third consecutive day. Doctors were puzzled and almost exhausted all options to stop this nasty bleeding from the nose. He took the journey from, after losing hopes, from Berber to Khartoum, not quite sure that his beloved son would make it. Dr. Faroog was in charge of the case. The child was admitted in the hospital, blood transfusions were made one bottle after another, and many tests were done.
– your son is confirmed to have a bleeding disorder, do you have any similar issues in the family? Asked Dr. faroog
-Yes, two of his uncles, mother’s brothers died at age of 9 and 13. Father replied.
-He is lucky to be born in an era that witnessed many improvements in the medical care of this clotting problem.
I was admitted at Khartoum Hospital for almost a week with the plasma infusion undertaken every 12 hours. the doctor assured there is a new medicine which would be a game changer in the lives of poor hemophiliacs. that was almost in 1971 when i was diagnosed and had my first treatment. My father and I came back to our home in the town of Berber, 360 Km north of the capital overwhelmed by the cheers of the relatives who presumed a miracle has been taking place and overloaded with many advice of the doctor on how to handle the case of boy. From that day i became a regular visitor to blood bank of Kh Hospital.
I went to the toilet, secretly wished to evaluate the efficiency of this medicine by myself. i was admitted because there was blood in my urine that lasted for couple of days. I came our rushing to my father, ” Yes, it is working dad, oh my God”.
What is working? asked my dad?
“The medicine” .i replied back………. “My urine turned to light yellow instead of red.”
it was a simple verification of the worthiness of the injected medicine. Color is changing from red to light yellow. i was stunned. my doubts turned into firm belief.
1976, i completed 10 years, with many self-awareness about the line that has been drawn. i sensed the attention of many eyes focusing on anything that i was doing. Playing football with my peers was a big taboo. I loved football and exhibited remarkable skills in playing. yet my friend would be very reluctant to let me play with them. They are afraid of the subsequences. At school the story was a bit different. The teachers were well informed about my case and warned that any physical punishment my lead to serious subsequences. I was very good at all subjects and topped the class. Not giving any teacher any reason to push me. Lashing the boys with whips was a common practice and the teachers were authorized to do it. when there a common punishment, the teacher would exclude me. some would make their own punishment for this strange boy. Mr. Amin, our math teacher, looked at me from face to toe and mockingly asked the class to stand up. it happened that i came late that morning and he was already in the classroom. He instructed the students to Welcome “His Highness” by singing the National Anthem. They did. He was so cruel to vent his anger in that way. i was down morally.
The same year, in the school holiday, my dad and i travelled to the capital by Half Express train. It was a privilege to travel to Khartoum, envied by my friends and give me times to narrate the wonders i have seen in Khartoum. They do not know that if it were not for this bleeding issues i would have never visited the capital. My wonder was that i had nothing this time to explain why we had to go to the capital. my health was great and no bleeding, being inside or outside.
The discussion was going on that morning with Dr. Faroog and some other big consultants providing more assurances to my dad that circumcision like any surgery would be efferently managed by the administration of the factor, factor 8.
Although i was cent per cent fit, i was admitted at the Pediatrics Section at the Hospital. Factor replacement was planned twice a day. My dad, noting the growing frustration inside me for being injected without a valid reason, he told me we planned to circumcise you. it is a simple procedure and there are no worries. I was a bit relived. Circumcision is something that relates to manhood in that closed environment. A man uncircumcised is not a man.
The day came. The news spread everywhere and our far and near relatives came to witness this “operation”. some of them, had no trust in the medicine at all, objecting seriously and surrendered to the will of my father who swear would never leave his son uncircumcised whatsoever. Three of the surgeons attended the surgery. Dr. Faroog set the hemostatic management plan with close monitoring of all essential parameters. After an hour i was pushed on a wheeled chair to the room. My aunts and other women ululated in joy. i spent around two weeks under the persistence of the medical team who left nothing for the chance. i was under the factor coverage for the entire period. Very minimal bleeding was observed. We returned to our hometown like a victorious army. when the train stopped at the station, we found a fleet of around 4 cars awaiting us. Celebration had to start and many cow blood were shed and many people were coming in to see the wonders, especially elders whom the occasion evoked their bitter memories of the earlier death of my two uncles.
My name is Ariel Yonatan Alin, I am 27 years old. I come from Surakarta, Central Java, Indonesia.
I am an individual with hemophilia A. I was detected with hemophilia when I was 6 years old, at that time I went to Sarjito Hospital Yogyakarta for treatment.
My experience dealing with hemophilia is very complex, because no one in my extended family suffers from hemophilia apart from me.
And I have overprotective parents.
The hardest experience was when I was little, I could only see my friends playing football.
Until I was an adult, I still regularly underwent treatment at the hospital, I was injected with factor 8 approximately once a week.
Currently I have completed my master’s degree in informatics, and hope to become a lecturer.
I hope that hemophilia treatment through genetic therapy can soon be implemented throughout the world, and at a much more affordable price.
#WHD #worldhemophiliaday #world #hemophilia #day #for #better #treatment
Hola, mi nombre es Lilly Villalon, soy de nacionalidad Mexicana y resido en Estados Unidos. Fui diagnosticada hace 2 años con Hemofilia A mild y VWD Type 2N, tengo un hijo de 17 años diagnosticado con Hemophilia A mild, y tengo 3 hijas que están en proceso de ADN 🧬 para checar si también tienen hemophilia.

Mi nombre es… Mateo naci en la ciudad de Trinidad, Beni-Bolivia, un 12 de abril del 2018, y actualmente vivo en San Ignacio de Moxos, una provincia del Beni.
Mi historia comenzó en San Ignacio de Moxos, en el mes de octubre del 2018, cuando tenia 6 meses de nacido.
La primera vez fue cuando un dia amaneci con un morete bajos mis axilas, mis padres pensaron que me habia lastimado con mi andador, la segunda vez me volvio aparecer otro morete en lado derecho de mi pecho, mis padres se empesaron a preocupar, por que ya no era nada normal, no entendia por que me salian los moretes, pensando que por accidente alguien de la familia me habria apretado muy fuerte, mi mama se preocupo mucho y me llevo con un medico particular, para saber el motivo por el cual me salian esos moretones, el doctor me reviso y le pregunto a mi mamá que si alguien me habia apretado o me habia alsado mal, hasta incluso penso que mis padres m golpeaban, a lo que mi madre respondio que no, que solo el morete habia aparecido de un momento a otro.
Entonces el doctor pidio unos analisis de laboratio, donde mi cuagulacion salio alterada, y pues nos envio a trinidad para una consullta con un pediatra, y el pediatra me reviso y llego a un diagnostico presuntivo de Hemofilia y como en trinidad no contamos con hematologo decidio enviarnos a la cuidad de Santa Cruz donde si cuentan hematologo, bueno despues de una consulta y varios estudios, m diagnosticaron con Hemofilia tipo b severa.
Una noticia muy impactante para mis padres, pero increiblemente tomaron con mucha calma la noticia, porque mi madre dijo que era una prueba que Dios puso en nuestras vidas, y confia en que nosotros podremos con la prueba siempre de la mano de Dios. Es una manera muy admirable de tomar la noticia,despues de tomarle la mano a mi padre y orar dandole las gracias a Dios por la vida, luego vi que mis padres lloraron cuando decidieron contar la noticia al resto de la familia, luego desde ese moemnto empezo mi vida con hemofilia, ahora tengo 6 añitos, y soy un niño bemdecido porque recibo tratamiento profilactico de fector IX, una gota de amor, vivo mi vida normal, no tengo problemas articulares, voy a la escuela y estoy en primero de primaria.
Realmente soy bendecido Dios cuida de mi, gracias a el estoy bien, y tengo una buena calidad de vida, dice mi madre que si yo me pongo a orar con el corazon y pido por mi sanidad, Dios me sanara, y sere un niño sano libre de Hemofilia.

My name is Novi Riandini, 50 years old. I am married to Muhammad Gunarso, who has Hemophilia B since 1998. At the beginning of our marriage, I encountered many difficulties finding information about Hemophilia. There were many things I didn’t know about how to care for a husband with hemophilia with limited treatment and medication options at that time.
Eventually, using my experience in Public Relations, I reached out to several doctors and parents of patients to establish a hemophilia community in Indonesia. Alhamdulillah, in the first 5 years, there was an increase in the number of diagnosed Hemophilia patients in Indonesia thanks to the media campaigns we conducted. Initially, only 98 people with hemophilia were recorded as diagnosed, but this year we have recorded almost 3000 hemophilia patients across Indonesia. We did a lot to educate the public, from holding seminars/trainings for medical professionals and the general public, sharing stories in print and electronic media, and many other PR campaigns.
The improvement in treatment and medication availability has also increased, balanced by government support through our national health insurance called BPJS.
Thank you, World Federation of Hemophilia and Indonesian Hemophilia Society.
Happy World Hemophilia Day, everyone.

I am Muhammad Gunarso, a 51-year-old Hemophilia B patient. I am the first diagnosed Hemophilia B patient in Indonesia, thanks to the assistance of the late Prof Djajadiman Gatot, MD. Since Indonesia joined the World Federation of Hemophilia, many changes have occurred in our country. Treatment, care, and government support for us have gradually improved. This is not without the hard work of the medical team at the Indonesian Hemophilia Society, who continuously advocate for hemophilia treatment in Indonesia. I also express profound gratitude to the WFH for their unwavering support through their Humanitarian Aid, which is always available and responsive when we need donated medication.
Pour toute question, veuillez contacter communications@wfh.org.